Frequently Asked Questions
Bronchoscopy
What is a bronchoscopy?
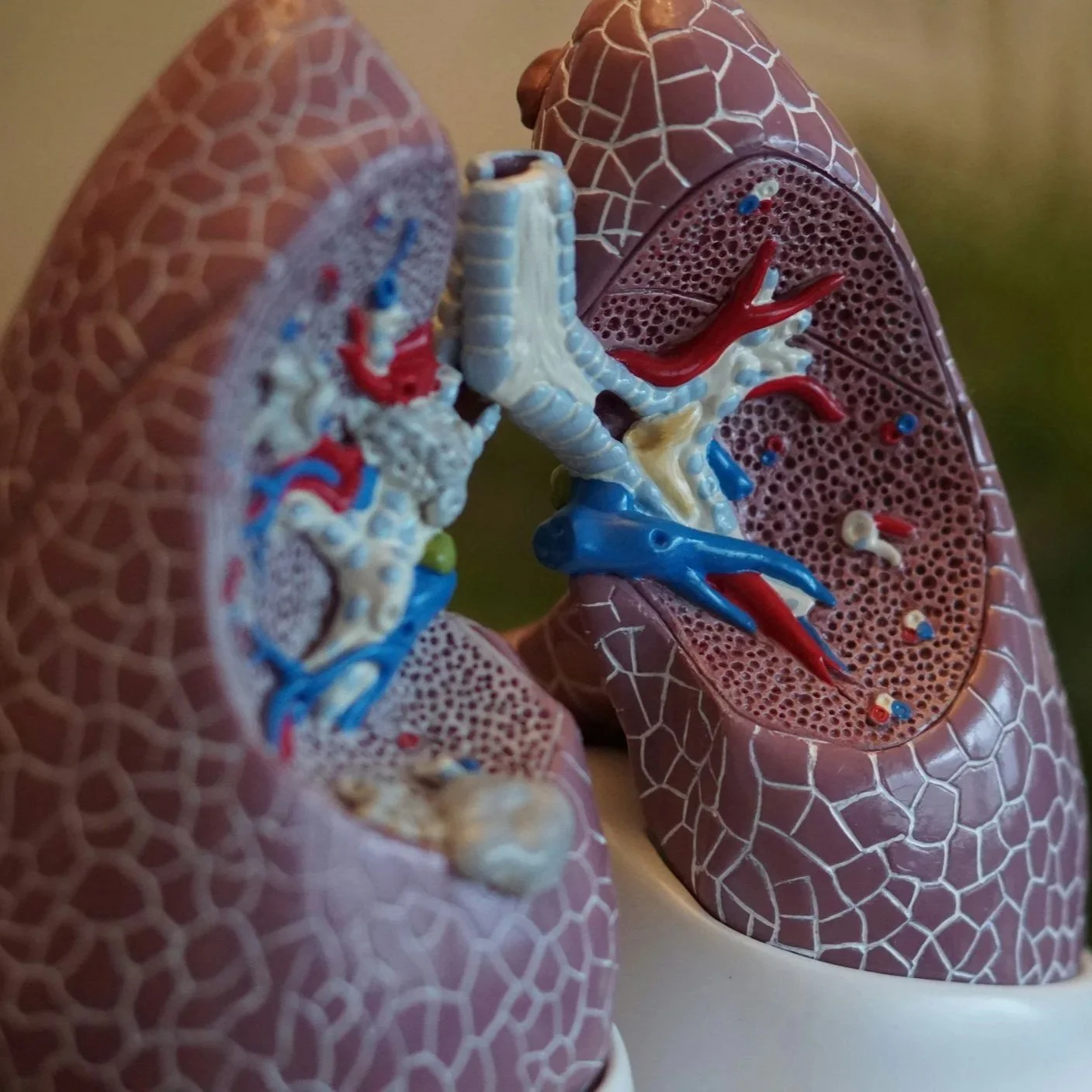
A bronchoscopy is a procedure that allows your doctor to look directly at your airways using a thin, flexible tube called a bronchoscope. It can help diagnose lung infections, tumors, chronic cough, or abnormal imaging findings.
Why do I need a bronchoscopy?
Persistent cough or abnormal chest X-rays/CT scans
Suspected lung infections or bleeding
Biopsy of lung tissue or lymph nodes
Evaluation of airway blockages or tumors
How do I prepare for the procedure?
Do not eat or drink for at least 6–8 hours before the procedure.
Inform your doctor about any medications you take, especially blood thinners.
Arrange for a ride home as you may be drowsy afterward.
Is it painful?
No. You’ll be given sedation or anesthesia to make you comfortable. You may have a sore throat or mild cough afterward.
How long does it take?
The procedure typically takes 30–60 minutes.
What are the risks?
Bronchoscopy is generally safe, but possible risks include bleeding, infection, low oxygen levels, or a collapsed lung (rare).
When will I get results?
If biopsies are taken, results are usually available in a few days to a week.
Thoracentesis
What is a thoracentesis?
A thoracentesis is a procedure to remove fluid from the space between the lungs and the chest wall (pleural space). It can help relieve shortness of breath and diagnose the cause of fluid buildup.
Why do I need this procedure?
Relieve pressure in the chest from excess fluid
Analyze the fluid to determine the cause (infection, cancer, heart failure, etc.)
How is it performed?
You will sit upright, and your doctor will numb the area between your ribs. A small needle or catheter is inserted into the pleural space to drain fluid.
Does it hurt?
You may feel a pinch and pressure, but the procedure is usually well tolerated under local anesthesia.
How long does it take?
About 15–30 minutes.
What are the risks?
Pain at the puncture site
Bleeding or infection
Rarely, a collapsed lung (pneumothorax)
Do I need to be hospitalized?
Most thoracenteses are done on an outpatient basis unless you're already hospitalized.
What happens after the procedure?
You may get a chest X-ray to ensure there are no complications. Resume normal activity as instructed.
Indwelling Pleural Catheter
What is an indwelling pleural catheter?
It’s a small, flexible tube placed in the chest to allow long-term drainage of fluid buildup around the lungs at home, often used for patients with recurrent pleural effusions.
Why do I need this?
If you have frequent fluid buildup from conditions like cancer, heart failure, or chronic inflammation, this catheter allows for easier at-home management and improves breathing.
How is it placed?
The catheter is placed under local anesthesia, typically during an outpatient procedure. A small incision is made to insert the tube, which is tunneled under the skin and secured in place.
Can I drain the fluid at home?
Yes. You or a caregiver will be taught how to drain the fluid using a sterile drainage kit.
How often should I drain it?
This depends on your symptoms and the amount of fluid. Most patients drain every 1–3 days.
Is it painful?
Some mild discomfort is expected initially, but it typically resolves within a few days. Pain control can be managed with medications if needed.
Can I shower with the catheter?
Yes, but you should keep the area dry and covered with a waterproof dressing. Avoid soaking or swimming.
How long does the catheter stay in?
It can stay in for weeks to months. In some cases, the catheter is removed if the fluid stops accumulating.
What are the risks?
Infection
Blockage of the catheter
Skin irritation or leakage around the site
When should I call the doctor?
f you develop fever, redness or swelling around the site, worsening shortness of breath, or if drainage becomes bloody or stops unexpectedly.